For bariatric surgery programs, the clinical procedure itself is often the most predictable part of the patient experience.
What’s far more complex – and far more fragile – is everything that happens before a patient ever reaches the operating room.
Across the U.S., bariatric surgery patients must navigate a lengthy, highly individualized preoperative journey shaped by insurance requirements, comorbidities, and multidisciplinary clinical clearances. This process can stretch for months, sometimes longer, and requires constant coordination between weight loss clinics, surgery departments, schedulers, coordinators, and referring providers.
At University of Alabama at Birmingham (UAB) Medicine, one of the Southeast’s flagship academic medical centers, leaders recognized that this complexity was creating unnecessary friction – for patients and for staff. Patients often felt confused about what they needed to complete and when. Care teams spent significant time on phone calls, chart reviews, and manual tracking just to keep patients moving forward. And like many bariatric programs nationwide, UAB had limited visibility into where patients were getting delayed… or dropping out altogether.
Rather than accepting this as “just how bariatrics works,” UAB asked a different question:
What if the journey to surgery could be as structured, transparent, and patient-centered as the surgery itself?
Bariatric surgery demand is rising, but so are expectations…
Despite the growing popularity of GLP-1 weight loss medications, bariatric surgery remains the most effective long-term treatment for patients with class III obesity. Demand for surgery continues to grow, while programs face increasing pressure to deliver:
- Faster time-to-surgery
- Higher patient retention
- Better patient experience
- Improved staff efficiency
For UAB, this wasn’t a hypothetical challenge. The health system already had firsthand experience using SeamlessMD across colorectal, thoracic, and gynecologic oncology surgery programs. Those deployments, fully integrated with the EHR and aligned with Enhanced Recovery protocols, had demonstrated that digital care journeys could meaningfully improve engagement, coordination, and outcomes at scale.
That existing foundation made bariatrics a natural next step.
Designing Digital Care Journeys for a Complex, Insurance-Driven Process
UAB launched two distinct digital care journeys to support patients and care teams across the bariatric continuum:
- Getting to Surgery:
This journey begins at the patient’s initial bariatric consult and continues until they are scheduled for surgery. It focuses on helping patients stay motivated and on track while completing insurance-driven requirements such as tests, assessments, and clearances. - Pre-Operative Preparation
Once patients are cleared, this journey prepares and optimizes them for surgery itself – delivering education, reminders, and guidance leading up to the procedure date.
Importantly, these were not generic “education apps.” They were purpose-built digital workflows designed to mirror the real operational and clinical steps of UAB’s bariatric program.
A Virtual Companion for Patients and a Workflow Engine for Care Teams
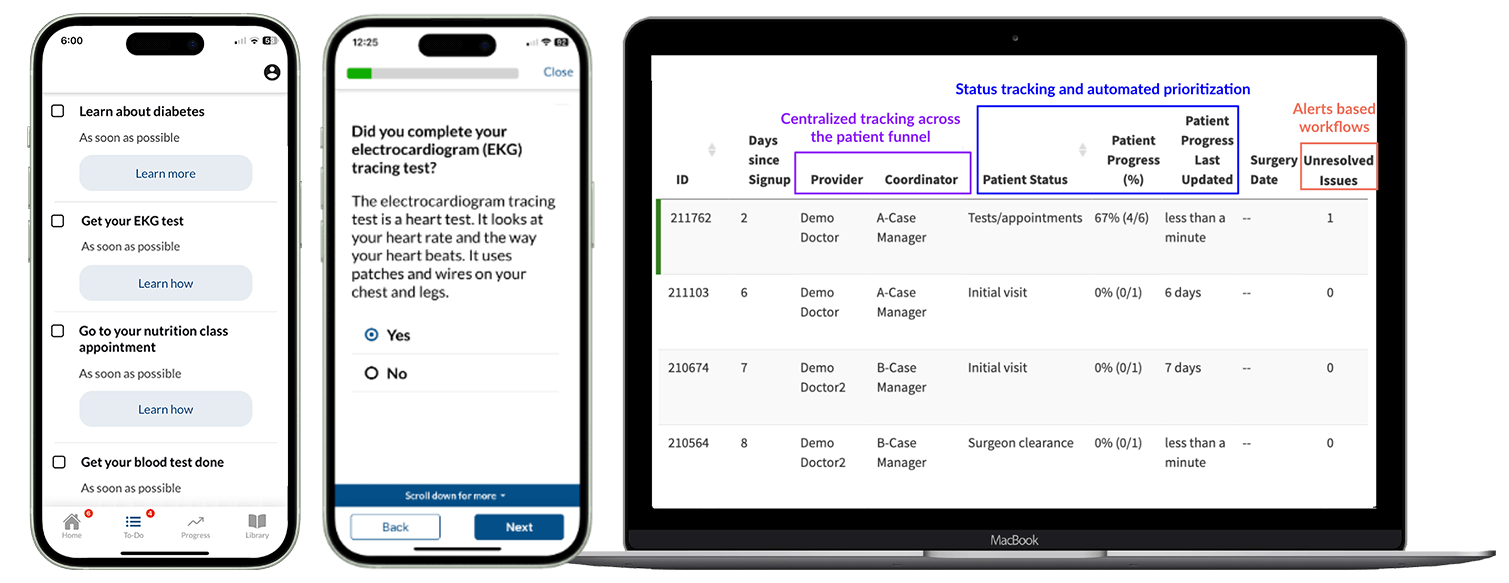
From the patient’s perspective, SeamlessMD functioned as a virtual companion throughout a long and often stressful process.
Patients received:
- A personalized, step-by-step to-do list tailored to their insurance requirements and health status
- Clear education explaining why each test, appointment, or clearance was needed
- Real-time visibility into where they were in the process, reducing uncertainty and anxiety
- An easy way to notify the care team when tasks were completed - or when help was needed
- Ongoing reminders and preparation guidance as surgery approached
For patients who might otherwise disengage or feel overwhelmed, this transparency proved critical.
On the operational side, the platform became a shared source of truth for the bariatric program.
Care teams gained:
- A shared dashboard used by both the Weight Loss Medicine Clinic and the Department of Surgery
- Centralized, real-time tracking of patient progress - eliminating manual spreadsheets
- Alerts when patients completed milestones or signaled a need for assistance
- Funnel-level visibility into bottlenecks, delays, and dropout points across the preoperative journey
For the first time, UAB could see not just that patients were delayed – but where and why.
Operational Impact: Less Chasing, More Care
The results were immediate and measurable.
After implementing SeamlessMD in bariatrics, UAB achieved:
- 5 minutes saved per patient message related to education and progress updates
- 80% reduction in daily staff phone calls (from ~30 per day to ~6)
- 71% of patients avoided phone calls altogether
- 15 minutes saved per patient in chart review time
For busy bariatric coordinators and clinical teams, these time savings added up quickly – freeing staff to focus on higher-value patient interactions rather than administrative follow-up.
Just as importantly, UAB gained real-time operational insight into:
- Patient dropout rates and timing
- Average time-to-surgery
- Time spent in each preoperative phase
- Specific tests or requirements that consistently created bottlenecks
This level of visibility is often the missing link between intent and improvement.
Empowering Patients While Improving Surgical Throughput
While early gains centered on efficiency, UAB sees broader downstream impact ahead.
By keeping patients informed, engaged, and moving forward, the program expects:
- Improved patient retention
- Shortened time-to-surgery
- More predictable surgical throughput in an increasingly competitive weight-loss landscape
Clinical leaders at UAB have seen the cultural shift firsthand.
“SeamlessMD has completely changed how we guide patients through their journey to bariatric surgery. Patients are empowered to be engaged through easy and convenient access to information and education. Our team has been able to streamline our workflow and improve both the efficiency of the bariatric surgery process and quality of the patient experience.”
— Christina Lundeen, BSN, RN, Bariatric surgery Clinical Care Coordinator, UAB
And from the surgical leadership perspective:
“SeamlessMD enables our patients to be active participants in their care. With the app they are able to track their progress, get help when they need it, and understand at all times where they are in the journey.”
— Dr. Richard Stahl, Director of Bariatric Surgery, UAB
A Model for Digital Transformation in Bariatric Care
For bariatric programs nationwide, UAB’s experience highlights a broader lesson:
Digital transformation isn’t just about postoperative monitoring or patient education libraries. It’s about operationalizing engagement across the entire care journey – especially in the most complex, insurance-driven phases where patients are most likely to disengage.
By combining patient-facing transparency with team-facing workflow intelligence, UAB turned one of bariatric care’s biggest challenges into a strategic advantage.
For administrators, bariatric leaders, and CMIOs looking to improve access, efficiency, and patient experience – without adding staff or burden – this approach offers a clear, scalable path forward.
Click here to read the full UAB Bariatric case study.
.svg)







.png)
