For quality and clinical operations leaders, the “alphabet soup” of CMS payment models is a constant reality. However, the upcoming Transforming Episode Accountability Model (TEAM) - launching January 1, 2026 - represents a significant shift. For more than 700 hospitals, this isn't an optional pilot; it’s a mandatory 30-day episode accountability framework for high-volume procedures, including joint replacements, hip fractures, spinal fusions, CABG and colorectal surgeries.
Under TEAM, hospitals are on the hook for the total cost and quality of care from surgery through 30 days post-discharge. The actual hospital stay is the biggest line item, eating up 60% to 80% of the budget, but much of that is "baked in" with OR and implant costs. The real headache is the variable costs - the "swing" factors like avoidable readmissions or SNF stays that decide if we stay in the black. Most of these risks hit after discharge. Success requires tightening inpatient efficiency while keeping a close eye on that post-hospital window.
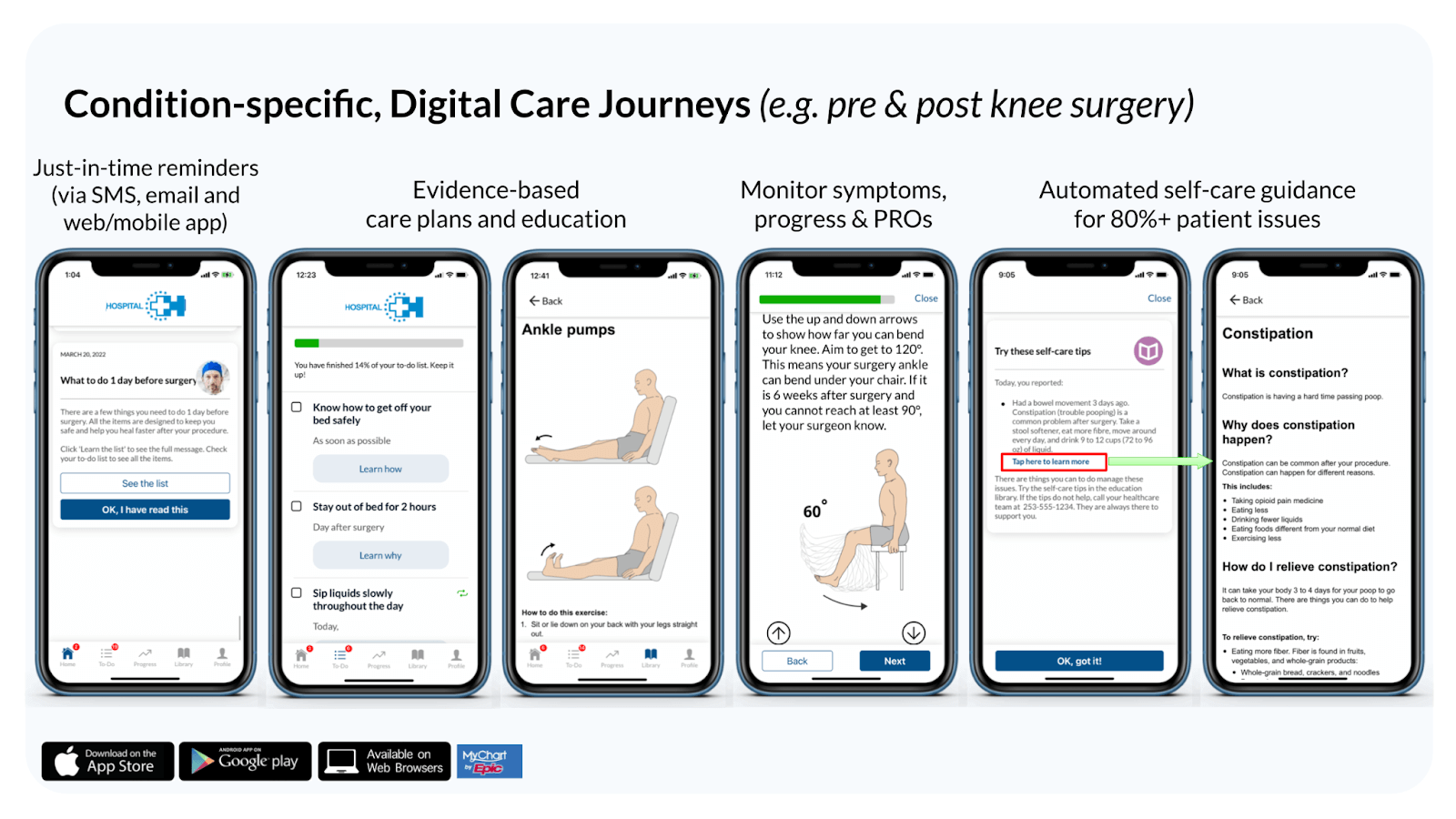
To manage these episodes effectively, many organizations are turning to Digital Care Journeys: these are digital platforms that guide patients through their entire surgical experience - from pre-op preparation to post-discharge recovery - using automated reminders, education, and remote symptom monitoring via the patient’s own smartphone or tablet.
Here are six strategies for using Digital Care Journeys to help health systems succeed under the TEAM model.
1. Standardize Care Pathways to Eliminate Cost Variation
One of the biggest hurdles in episode-based models is clinical variation. When every surgeon has a different set of pre-op instructions or post-op milestones, costs and outcomes become unpredictable.
A Digital Care Journey allows a health system to digitize its “gold standard” clinical pathways (e.g. ERAS). The platform ensures every patient receives the same evidence-based education and preparation. When patients are guided through a standardized prehab and ERAS program, they arrive for surgery better prepared and adhere to proven post-op recovery protocols, which leads to more predictable - and less costly - surgical outcomes.
2. Support Aggressive Reductions in Length of Stay (LOS)
Since the initial hospital stay accounts for 60% to 80% of the total episode spend, reducing LOS by even half a day across hundreds of episodes can significantly move the needle on financial performance.
Digital care journeys support this by reinforcing Enhanced Recovery After Surgery (ERAS) protocols directly to the patient. By providing daily "to-do" lists - such as early mobilization goals and incentive spirometry reminders - the technology keeps patients on track in real-time. When patients are active participants in their own recovery, they often meet discharge criteria faster and feel more confident leaving the hospital, knowing they have a digital guide for the next phase.
Moreover, when patients know they are being supported and remotely monitored after discharge via these digital platforms, they are more confident to be discharged 0.5 to 1 day earlier.
For example, click here to see how Atrium Health used digital care journeys to reduce LOS by 1 day for colorectal surgery.
3. Transition More Patients Directly to Home
Post-acute spend is a primary determinant of episode savings. While post-acute care historically represents roughly 15% to 25% of the 30-day episode cost, it is the area with the most discretionary variation. Hospitals have a clear financial incentive to safely transition as many patients as safely possible directly to their homes rather than high-cost Skilled Nursing Facilities (SNFs).
The primary reason patients push for a SNF is fear of the unknown. Digital Care Journeys act as a virtual safety net, providing a "connected" experience that bridges the gap between the hospital and the home. By providing the clinical team with a way to monitor recovery data remotely, the hospital can safely discharge patients to their homes, knowing that if a red flag appears - such as uncontrolled pain or a suspicious wound - the system will alert the care team for early intervention.
4. Use “Deviceless” Monitoring to Prevent Readmissions
Readmissions are a major financial risk in the TEAM model, often costing a hospital $12,000 to $15,000 per event. Many 30-day readmissions are for manageable issues - dehydration, minor surgical site infections, or medication confusion - that could have been handled in an outpatient setting if caught early.
While some look at device-based Remote Patient Monitoring (RPM) using hardware like blood pressure cuffs, "deviceless" journeys are often more effective for surgical episodes. Patients are much more likely to engage with a simple app on their phone that asks, "what is your pain today?” than they are to manage a suite of external hardware. For health systems, deviceless digital care journeys are more economically scalable to thousands of patients, while cost-heavy device RPM platforms often can only be afforded for dozens of patients at a time.
Deviceless, digital care journey platforms like SeamlessMD allow clinicians to catch these small issues through automated digital symptom checks, preventing a minor complication from escalating into an expensive Emergency Department visit.
For example, click here to learn how Baystate Health used digital care journeys to reduce readmissions by 72% for CABG.
5. Automate the Collection of PROMs
Success in the TEAM model isn't just about saving money, it’s about hitting quality targets. CMS is doubling down on Patient-Reported Outcome Measures (PROMs). For joint replacements (THA/TKA), capturing these metrics is a requirement for the model.
Manually collecting PROMs via phone calls or mail is labor-intensive and results in low response rates. Digital Care Journeys automate this process by prompting patients to complete surveys (like the HOOS, JR. or KOOS, JR.) at the exact intervals required by CMS. By integrating these surveys into the patient’s daily recovery journey, response rates are significantly higher, ensuring health systems meet the quality thresholds necessary to retain their reconciliation payments.
6. Close the Loop with Primary Care Referrals
A unique requirement of the TEAM model is the mandate for hospitals to refer patients to primary care services. CMS wants to ensure that a 30-day surgical episode leads back into a long-term, accountable care relationship. With physician fees making up approximately 13% to 19% of episode costs, efficient outpatient coordination is vital.
Digital platforms help facilitate this transition by reminding patients of the importance of their primary care follow-up and prompting them to confirm they’ve scheduled an appointment. By closing this loop, hospitals can reduce the fragmentation that often leads to poor long-term outcomes, ensuring that the progress made during the 30-day surgical episode is sustained.
Preparing for 2026
The CMS TEAM model is a clear signal that the era of fragmented surgical care is coming to an end. As 2026 approaches, the health systems that thrive will be those that extend their reach beyond the four walls of the hospital.
By leveraging Digital Care Journeys, hospitals can empower patients to be active participants in their recovery, give clinicians the data needed to intervene early, and deliver the high-value, cost-effective care that the TEAM model demands. The time to build that digital infrastructure is now.
.svg)






.png)
